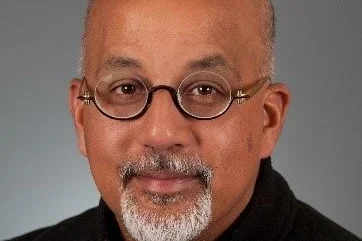
UCLA Faculty Spotlight: Striving for reproductive health equity in challenging times

Dr. Aparna Sridhar, MD, MPH, is a Professor of Clinical Obstetrics and Gynecology at UCLA’s DGSOM. Passionate about medical education, she has a special interest in incorporating technology into patient and physician education. Her training both internationally and in the United States gives her a deep understanding of cultural influences on healthcare.
GHP interviewed Dr. Sridhar to learn more about her work in reproductive health equity.
GHP: How do you define global health equity in the context of women’s reproductive health, and why is it important?
Dr. Sridhar: Reproductive health needs begin before the onset of menstruation to well beyond menopause. It encompasses many components, including but not limited to menstrual health, maternal care, gynecological care, and menopausal support. Equitable access to these services is not only a matter of reproductive justice but also closely linked to overall health outcomes and quality of life.
Achieving global health equity requires a focused commitment to addressing systemic barriers, cultural stigma, and geographical limitations that disproportionately affect access to care.
GHP: What drew you to work in global health equity with a focus on women’s reproductive health?
Dr. Sridhar: My interest in health equity began during my formative years of medical education in a small town in southern India. During medical school, I witnessed firsthand the profound impact of socio-economic and geographic disparities on health outcomes. The urban tertiary hospital where I trained served as a referral center for the surrounding rural areas, bringing into sharp focus how a person's zip code and financial capacity dictated their access to and quality of care. Most patients in our facility, particularly women, were economically disadvantaged and completely relied on government-issued health benefits, often insufficient to cover comprehensive reproductive healthcare. During my clinical work in obstetrics in medical school, I observed that women bore a disproportionate burden of preventable health complications due to delayed care, cultural norms, and economic barriers. These reproductive health challenges were further exacerbated by limited access to contraception, safe abortion services, and comprehensive maternal care, all of which are necessary for reproductive health equity. The preventable maternal deaths and near misses I witnessed highlighted the gendered and systemic barriers to equitable healthcare.
Following medical school, I immigrated to the United States. I was hopeful that advanced education in Obstetrics and Gynecology in a high-resource country with greater reproductive autonomy for women would deepen my learning context. However, I was shocked to encounter significant inequities within the U.S. healthcare system. While the context was different, the underlying disparities rooted in socio-economic status, race, and geographic location were alarmingly similar. This realization deepened my determination to focus my professional life on addressing social determinants of health both locally and globally, from education and economic empowerment to political advocacy for equitable healthcare policies. I am committed to a world where every woman, regardless of where she lives, has access to safe, affordable, and comprehensive reproductive healthcare.
GHP: What support structures are most critical for ensuring the ongoing health and well-being of women in underserved communities, particularly in communities with high maternal mortality rates?
Dr. Sridhar: An average woman spends about one-third of her reproductive life requiring maternal health services if she chooses to have children and two-thirds managing menstrual health and other reproductive needs. Viewing reproductive health as a continuum of care, it is important to establish a strong foundation before menarche that extends beyond menopause. I have identified the top 5 factors that are critical to ensure comprehensive maternal and reproductive health care for women, regardless of their social background. Addressing these factors holistically is vital to bridging healthcare disparities and advancing reproductive health equity globally.
- Trust in the health care system: A fundamental factor influencing effective reproductive care is the individual’s and community's trust in the healthcare system. For reproductive health services to be truly impactful, individuals and communities must have confidence in their health system’s accessibility, quality, and fairness. The health system should also be aligned with the cultural values of that community. Building this trust requires consistent, culturally sensitive care and transparent communication.
- Access to comprehensive healthcare services: Every community deserves access to comprehensive maternal care facilities that provide antenatal services, skilled birth attendants, emergency obstetric care, and postpartum support. This care must be complemented by comprehensive family planning and reproductive health services, including education, counseling, and consistent follow-up care.
- Community involvement and male engagement: Male partners and the communities surrounding women can play an important role in helping women to address cultural barriers. Working with these groups will foster a supportive environment for women’s health and autonomy.
- Supportive legal and policy work: Advocacy for policies that protect women’s rights to reproductive health services will make a huge difference in providing access to care. The policies should be based on data collected and analyzed to help identify gaps, monitor progress, and allocate resources effectively to reduce maternal mortality rates. Working with Health Ministries and policymakers is key.
- Trained healthcare workforce: Training and retaining physicians, skilled birth attendants, midwives, and community health workers (CHWs) is essential for improving maternal health outcomes. Healthcare professionals with insufficient training can inadvertently perpetuate myths and mistrust within communities and may significantly increase the risk of maternal deaths if they are not prepared to handle emergency situations effectively. Ensuring that all healthcare providers are well-equipped with the necessary skills and knowledge key.
GHP: What are some of the programs or initiatives you’ve been involved in that have made a tangible difference in improving access to women’s reproductive healthcare?
Dr. Sridhar: Throughout my professional journey, I have constantly asked myself: "What can I do at a personal and professional level to prevent maternal mortality and promote equitable reproductive healthcare for women globally?" Among the five critical support structures I identified earlier, I realized that I could have the greatest impact by strengthening the healthcare workforce and building trust in the community. This has meant focusing on training providers and educating communities with accurate, evidence-based medical information to build trust in the available interventions.
After solidifying my medical knowledge and clinical skills, I pursued an MPH to deepen my understanding of health education and promotion. During this time, I also completed advocacy training, which proved invaluable in grasping how policy changes and legal frameworks can be leveraged to benefit patients. I have since dedicated my efforts to bridging gaps in provider and patient education using technology, transcending geographical borders to ensure that accurate reproductive health information and training reach even the most underserved communities. This focus on education and technology has become my niche in advancing global health equity.
My global health research is centered on advancing reproductive health equity, particularly in contraception, family planning, and maternal health. In my early research, I focused on leveraging technology to disseminate evidence-based reproductive health information effectively. This involved developing educational tools like mobile health applications, games, and comics to improve health literacy and decision-making, especially for low-literacy populations across geographical boundaries.
In recent years, my efforts have expanded to include meaningful collaborations with professional organizations such as the American College of Obstetricians and Gynecologists (ACOG) and the International Federation of Gynecology and Obstetrics (FIGO). Through these partnerships, I have worked on enhancing evidence-based education for the global healthcare workforce. One of my significant projects with FIGO is the Contraception Mapping Project, funded by the Gates Foundation, where I led initiatives to assess and broaden contraceptive access across 74 member countries. This project has been instrumental in identifying gaps and implementing strategies to improve reproductive health services globally. In another project, we are using virtual simulation training on Obstetrical Emergencies with the South Asian Federation of Obstetrics and Gynecology. This will be training the future obstetricians in the south Asian region to be more prepared for emergency situations. Overall, my work aims to bridge healthcare disparities by integrating technology, education, and policy advocacy, ensuring equitable access to comprehensive reproductive healthcare for women worldwide.
GHP: How do political changes or funding cuts affect your ability, and the ability of your colleagues, to provide care and advocate for women’s health?
Dr. Sridhar: In recent weeks, I have observed the profound impact of funding cuts resulting from recent political changes in the United States. For instance, the full implications of the U.S. withdrawal from the World Health Organization (WHO) are still unfolding, posing significant risks to global reproductive health initiatives. Similarly, substantial reductions to USAID funding have led to the abrupt cessation of numerous projects where I was a contributing member of the team.
Unfortunately, political interference in women's reproductive health is not a new challenge. Reproductive and maternal health services have a longstanding history of being undermined through the dismissal of evidence-based medicine, the criminalization of essential services, and the imposition of medically unnecessary restrictions. These actions not only compromise the quality of care but also erode the trust between patients and providers.
Despite these challenges, our commitment to providing comprehensive care and advocating for women's health remains steadfast. We will continue to seek alternative resources for our programs and research, ensuring that the essential work of advancing reproductive health does not come to a halt. No political obstacle will deter our efforts to support women's health and rights locally and globally.
GHP: What advice do you have for trainees who want to make a meaningful impact in women’s* reproductive health despite the current challenges?
Dr. Sridhar: My advice to trainees is to remain committed and resilient despite the ongoing challenges. While political climates may shift, our commitment to evidence-based science must remain unwavering. It is essential to maximize the impact of available resources by focusing on innovative solutions and maintaining a data-driven approach to care. I encourage trainees to have an open mind and become advocates for women's reproductive rights and autonomy. It is important to engage our trainees early on in their medical career so that regardless of the specialty they choose, approaching healthcare with a lens of reproductive justice will significantly enhance the quality of care provided to women. Understanding the intersections of reproductive health within broader social determinants is vital for ensuring equitable access and outcomes.
Active involvement in professional organizations and their advocacy efforts is another crucial step. By participating in these networks, trainees can amplify their voices, stay informed about policy changes, and contribute to collective efforts aimed at safeguarding reproductive health rights.
Lastly, cultivating skills in policy advocacy, health education, and cultural competency will prepare trainees to lead effectively in any field, including in reproductive health. The challenges are many, but the need for dedicated providers who can champion reproductive justice has never been more critical.
*As language around gender continues to evolve in the scientific and medical communities, we will use the terms "woman" and "women" and the pronouns "she" and "her" in this presentation. However, this is not intended to exclude individuals who have a uterus but do not identify with these terms.